No products in the cart.

Continuous Glucose Monitoring (CGM) is a revolutionary approach that enables people with diabetes to monitor their glucose levels throughout the day and night in real time. It is a system that allows people with diabetes to detect trends and patterns in their glucose levels. Instead of using blood like a traditional blood glucose meter, this system uses interstitial fluid (the clear fluid surrounding your body’s cells) to determine a glucose value. Interstitial fluid mimics the same trends that blood glucose does.
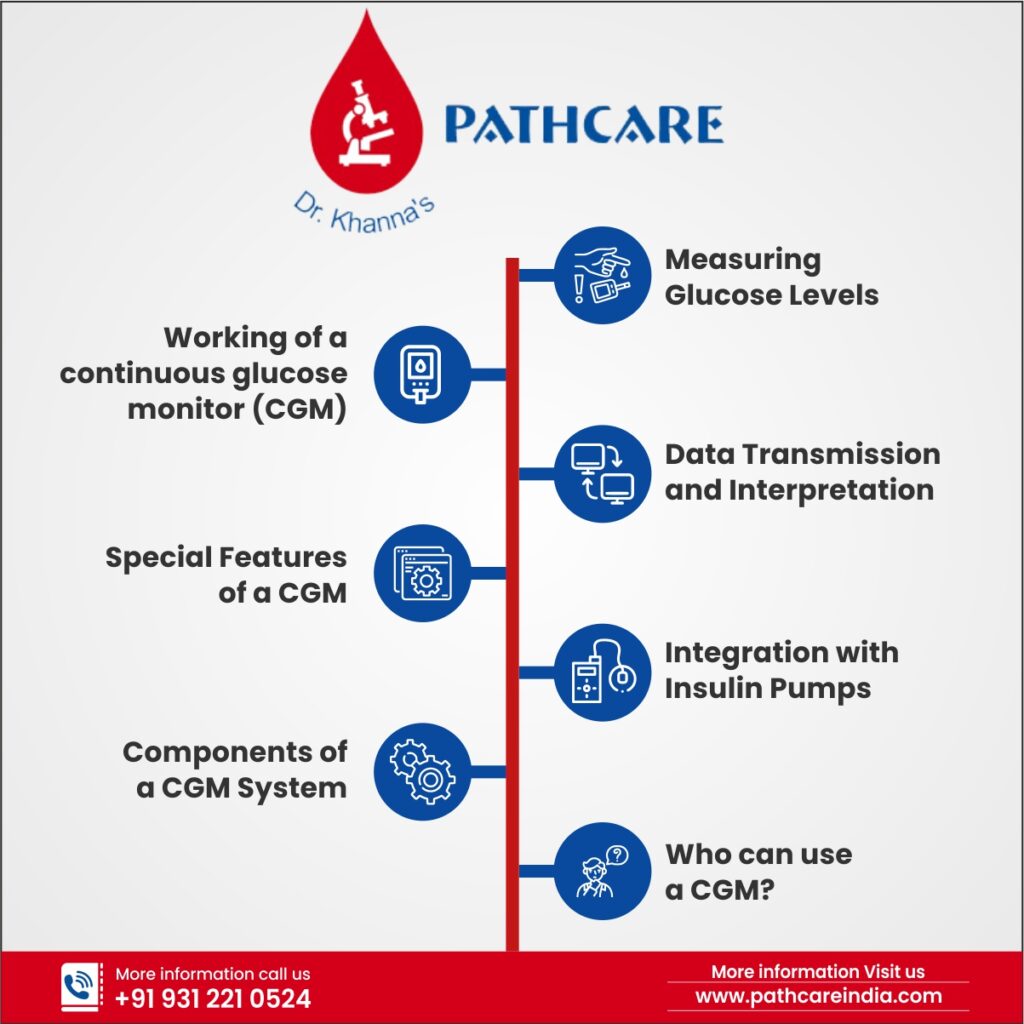
Working of a continuous glucose monitor (CGM)
A CGM works through a tiny sensor inserted under your skin, usually on your belly or arm. The sensor measures your interstitial glucose level, which is the glucose found in the fluid between the cells. The sensor tests glucose every few minutes. A transmitter wirelessly sends the information to a monitor.
The monitor may be part of an insulin pump or a separate device, which you might carry in a pocket or purse. Some CGMs send information directly to a smartphone or tablet.
Special Features of a CGM
CGMs are always on and recording glucose levels—whether you’re showering, working, exercising, or sleeping. Many CGMs have special features that work with information from your glucose readings:
- An alarm can sound when your glucose level goes too low or too high
- You can note your meals, physical activity, and medicines in a CGM device, too, alongside your glucose levels
- You can download data to a computer or smart device to see your glucose trends.
Some models can send information right away to a second person’s smartphone—perhaps a parent, partner, or caregiver. For example, if a child’s glucose drops dangerously low overnight, the CGM could be set to wake a parent in the next room.
Components of a CGM System
A real-time continuous glucose monitoring CGM system comprises three main components:
#1. Sensor
This is a tiny electrode inserted just beneath the skin, typically on the abdomen or upper arm, and it measures glucose levels in the interstitial fluid. The sensor is typically encased in a small, flexible, and water-resistant housing.
#2. Transmitter
Attached to the sensor, the transmitter is responsible for wirelessly sending glucose data to the display device. It converts the sensor’s readings into electrical signals and transmits the information using Bluetooth or other wireless communication protocols.
#3. Display Device
This can be a dedicated CGM receiver, a smartphone, or a smartwatch that receives and displays real-time glucose data. The display device often features customizable alarms and alerts to notify users of potential glucose excursions.
Measuring Glucose Levels
The sensor measures glucose levels in the interstitial fluid, the fluid that surrounds body cells. Interstitial glucose levels closely correlate with blood glucose levels, making it a reliable indicator of blood sugar status.
The sensor is coated with a biocompatible material that reacts with glucose, generating a small electrical current. The strength of this current is proportional to the glucose concentration in the interstitial fluid.
Data Transmission and Interpretation
The transmitter continuously collects data from the sensor and sends it to the display device every few minutes, providing a real-time glucose graph.
This allows users to view their current glucose levels and trends, which can help them make informed decisions about insulin dosing, diet, and exercise.
Many CGM systems also include predictive algorithms that analyze glucose trends to estimate future glucose levels. These predictions can help users take proactive measures to prevent potential high or low-glucose events.
Integration with Insulin Pumps
Some CGM systems can communicate directly with insulin pumps, forming an integrated system known as a sensor-augmented pump (SAP).
This integration allows the insulin pump to receive real-time glucose data and adjust insulin delivery accordingly. Advanced systems, such as hybrid closed-loop systems, combine CGM and insulin pumps to automate insulin delivery partially or entirely, significantly reducing the burden of diabetes management.
A continuous glucose monitoring system works by using a sensor to measure glucose levels in the interstitial fluid, transmitting this data to a display device for real-time analysis, and integrating it with insulin pumps for better diabetes management.
By understanding the technology behind CGM systems, individuals with diabetes can better appreciate the benefits it brings to their daily lives.
The benefits of a Continuous Glucose Monitoring system are as follows: –
#1. Improved Diabetes Management
A CGM system senses and records your glucose levels every 5 minutes, which means it can show real-time trends – whether they are rising or falling. In contrast, blood glucose meters provide you with only a measurement (or “snapshot”) of your blood glucose levels at a particular point in time. So, with blood glucose meters, you can take corrective action only after you learn of a high or low reading. However, with a CGM system, you can see the trend in your glucose level as they develop.
#2. Better Glycemic Control
Continuous glucose monitoring has been shown to improve glycemic control, as measured by reductions in HbA1c levels, in both type 1 and type 2 diabetes patients. Better glycemic control can help reduce the risk of long-term complications associated with diabetes, such as heart disease, kidney failure, and vision problems.
#3. Reduced Hypoglycemia Risk
CGM systems can alert users when their blood sugar levels are dropping too low, helping them take appropriate action to prevent hypoglycemia. Hypoglycemia, or low blood sugar, can cause symptoms such as dizziness, confusion, and even loss of consciousness, making its prevention crucial for people with diabetes.
#4. Reduced Diabetes-Related Stress
Living with diabetes can be stressful, thus constant monitoring of blood sugar levels and making treatment decisions can take a toll on mental health. CGM systems can help reduce this stress by providing continuous, real-time information on glucose levels, allowing people with diabetes to feel more in control of their condition.
#5. Increased Confidence and Independence
With continuous glucose monitoring, individuals with diabetes can gain a better understanding of how their bodies react to different foods, activities, and insulin doses. This increased knowledge can lead to greater confidence in managing diabetes and a greater sense of independence.
Drawbacks and Considerations
#1. Cost
Continuous glucose monitoring systems can be expensive, and not all insurance plans may cover the cost of the device and supplies. It is essential to consider the financial aspects and check with your insurance provider before investing in a CGM system.
#2. Sensor Accuracy
While CGM sensors have improved in accuracy over the years, they may still occasionally provide inaccurate readings. It is important to follow the manufacturer’s guidelines and calibrate the sensor as needed to ensure the most accurate results.
#3. Skin Irritation
Some people may experience skin irritation at the sensor insertion site. If you have sensitive skin or allergies to adhesives, consult with your healthcare provider for guidance on minimizing irritation.
Who can use a CGM?
Most people suffering from type 1 diabetes can use CGMs. Research is underway to learn how CGMs might help people with type 2 diabetes.
CGMs are approved for use by adults and children with a doctor’s prescription. Some models may be used for children as young as 2 years. Your doctor may recommend a CGM if you or your child:
- are on intensive insulin therapy, also called tight blood sugar control
- have hypoglycemia unawareness
- often have high or low blood glucose
Your doctor may suggest using a CGM system all the time or only for a few days to help adjust your diabetes care plan.